Highlights – Vitamin D and COVID-19 in a nutshell:
- Low vitamin D status is associated with cardiovascular disease, hypertension, metabolic syndrome, and obesity, and researchers are beginning to ask if it is also associated with more severe COVID-19 illness.
- Vitamin D deficiency/insufficiency is common, particularly in the elderly, dark skinned people, overweight/obese, people in northern latitudes, and people who avoid sunlight.
- Vitamin D has several mechanisms of action that are relevant to SARS-CoV-2 (affects the innate and adaptive immune response, dampens inflammation, suppresses the renin-angiotensin system, increases ACE2, reduces DPP4, and has many impacts on coagulation).
- Identifying and fixing vitamin D deficiency/insufficiency is good for general health and is easy, inexpensive, and safe to do.
The COVID-19 pandemic continues to impact the globe, and while the number of daily new cases is starting to come down in some areas, it is rising in others. A lot of effort has been made to prevent the spread of illness through stay at home orders and social distancing, and many trials are underway to find potential cures mainly through repurposing old drugs, like Remdesivir, hydroxychloroquine and various antivirals, among others. However, because SARS-CoV-2 is an RNA virus prone to mutations, it is likely that we will be dealing with the virus for some time. In fact, it has been proposed that like we have a flu season, we may now also have a COVID season that we will need to contend with. And so, another way that we can address this situation is to look at what we can do to build our health so that we are less likely to have a severe course of disease should we become infected. It is known that risks for severe COVID-19 illness include advanced age, hypertension, cardiovascular disease, diabetes, obesity1, as well as male sex2. However, some researchers have asked the question whether poor vitamin D status is also a risk factor3–5.
Vitamin D and Respiratory Tract Infections
Vitamin D is best known for its role in calcium homeostasis and bone metabolism; however, vitamin D receptors (VDR) have been found throughout the body, including on immune cells, indicating that it plays a role in our immune function. In fact, numerous studies have looked at the relationship between vitamin D and infectious diseases. For example, we talk about “flu season”, which is primarily in the winter, and corresponds to reduced sun exposure6 and typically lower vitamin D levels7, since vitamin D is synthesized in the skin from sun exposure. A randomized, double-blind, placebo controlled study showed that daily supplementation of 1200 IU of vitamin D3 compared to placebo in 334 schoolchildren reduced incidence of influenza A by 50%8. A systemic review and meta-analysis concluded that vitamin D supplementation provided an overall protection from respiratory tract infections, particularly in people who had extreme vitamin D deficiency and when taken in regular rather than bolus doses9.
The results of studies looking at vitamin D supplementation to prevent or reduce the disease burden of the flu and common cold have been mixed. This might be because the benefit of vitamin D supplementation is most pronounced in people with insufficient or deficient levels, whereas less benefit may be seen by supplementation in people with already sufficient levels9. Therefore, baseline levels of vitamin D status are important but have generally not been considered in these studies, which may obscure the positive impact of vitamin D supplementation.
Vitamin D may also protect against the potential complications of the flu and respiratory tract diseases, like pneumonia and acute respiratory distress syndrome (ARDS), both of which are also complications of COVID-19. A meta-analysis of observational studies found a 64% increased risk of community acquired pneumonia in people with vitamin D levels of less than 20 ng/mL10. Observational studies do not prove causation; however, this shows that people with low vitamin D levels appear to be at greater risk of developing pneumonia.
Vitamin D and ARDS
Hyperinflammation and cytokine storm are a feature of severe COVID-19 cases, and cytokine storm is a major cause of ARDS11. Vitamin D deficiency also appears to increase the risk of developing ARDS12, which is commonly treated with oxygen support, including. A study that used high doses of vitamin D compared to placebo in patients requiring ventilation in the ICU showed that a total vitamin D dose of 500,000 IU (100,000 IU per day for 5 days) and 250,000 IU (50,000 IU per day for 5 days) significantly reduced the length of hospital stay to 18 and 25 days, respectively, compared to 36 days in patients taking placebo13.
Vitamin D Status in COVID-19 patients
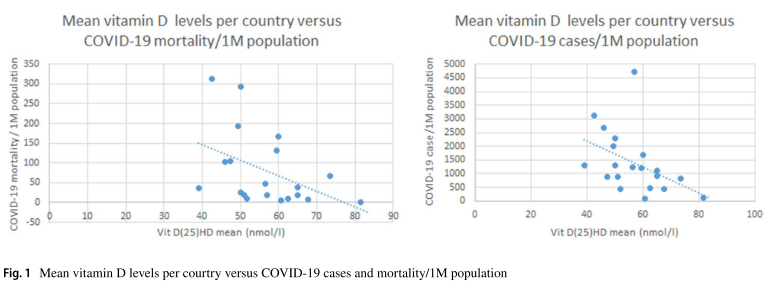
So, the question is whether vitamin D status plays a role in rates of infection or mortality in COVID-19 patients. Just because there seems to be a relationship with vitamin D levels and other infectious diseases, we cannot assume it will be so with SARS-CoV-2, since it is a new virus with different mechanisms. There have been a few epidemiological studies looking at vitamin D levels, latitude, and rates of infection and mortality. Rhodes et al. pointed out that here appears to be reduced mortality in latitudes under 35°, and they note that 35° North “also happens to be the latitude above which people do not receive sufficient sunlight to retain adequate vitamin D levels during winter”14. Ilie et al. plotted the mean levels of vitamin D for 20 European countries against incidence of COVID-19 mortality and infections and identified an inverse relationship (see the figure below)15.
However, latitude is not the only variable in vitamin D status. In a preprint (a publication that has not yet been peer-reviewed), Lau et al. discuss the differences in COVID-19 outcomes between different communities. In Louisiana, for example, African Americans make up 32% of the population but account for 70% of COVID-19 deaths; whereas a Boston homeless shelter had an outbreak of 147 cases of COVID-19, all of which were asymptomatic16. They write, “The mechanisms underlying severe COVID-19 should account for both these findings, as well as other COVID-19 mortality risk factors: hypertension, obesity, male sex, advanced age, concentration in northern climates, and COVID-19 associated coagulopathy (CAC),” and they assert that vitamin D insufficiency “meets every one of the above criteria.” They explain that vitamin D is common in people with darker skin, and while nutrition status is generally low in the homeless population, vitamin D status might be less of a nutrient of concern because of more sunlight exposure as a result of spending more time outdoors.
Over one billion children and adults are vitamin D deficient or insufficient, which makes it a global health issue17. The Endocrine Society Practice Guidelines define vitamin D deficiency as a serum 25(OH)D level of <20 ng/mL, insufficiency as a 21-29 ng/mL, and sufficiency as at least 30 ng/mL. People of color, pregnant women, obese people, and the elderly are populations commonly deficient in vitamin D. In addition, low vitamin D status commonly accompanies conditions like metabolic syndrome, diabetes, cardiovascular disease, and hypertension. In short, many of the risk factors for severe COVID-19 illness in and of themselves are associated with low vitamin D status.
The Role of ACE2 in COVID-19
Hypertension or high blood pressure is one of the risk factors for severe COVID-19 illness, and it is also associated with low vitamin D status. Vitamin D suppresses the renin-angiotensin system (RAS)18, which is an elaborate feedback loop involving the liver, lungs, kidneys, adrenal and pituitary glands and blood vessels that regulate blood pressure, among other things. The RAS system has been getting a lot of attention because it includes an enzyme called ACE2, which is actually the target of the SARS-CoV-2 virus.
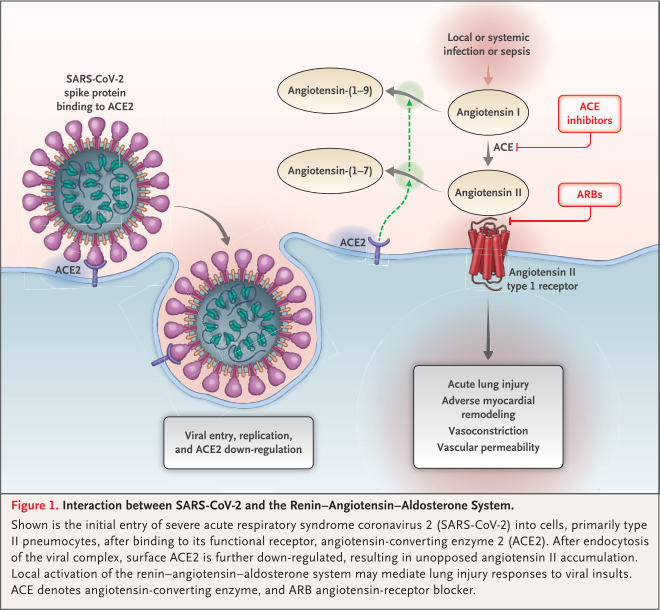
As the illustration19 shows, the virus docks to the ACE2 protein, which allows the virus to be transported into the cell via a process called endocytosis. Once inside the cell, the virus hijacks the cell’s components used to replicate genetic material, and that is how the virus replicates. In the process of doing this, the ACE2 levels go down.
ACE2 plays an important role in converting angiotensin II to angiotensin (1,7). Angiotensin II raises blood pressure through a variety of mechanisms, one of which is through vasoconstriction. Its actions are what the common hypertension drugs ACE inhibitors (e.g. Lisinopril) and ARBs (e.g. Losartan) are targeting to reduce blood pressure. Angiotensin II also increases oxidative stress and can cause lung injury. ACE2 counterbalances angiotensin II by converting it to angiotensin (1,7), which dilates the blood vessels, has an anti-hypertensive effect and is anti-inflammatory. When ACE2 levels are low, angiotensin II activity is high and may one of the mechanisms thought to contribute to the hyperinflammation seen in COVID-19.
Vitamin D has been shown to suppress the renin-angiotensin system and also increase the expression of ACE220. Overall, these actions should help reduce blood pressure and inflammation; however, because ACE2 is also the target of SARS-CoV-2, it is possible that higher ACE2 levels will increase susceptibility to infection. It is unclear whether the benefit of ACE2 and its anti-inflammatory action outweighs its role in the pathogenesis of infection with this virus. This question remains to be answered. However, it is noteworthy that ACE inhibitors and ARBs, which also increase the expression of ACE2, are being investigated as potentially protective in COVID-19. (You can read more about that here.) In an animal study looking at the role of ACE2 in SARS, caused by the SARS-CoV virus which also targets ACE2, the authors conclude, “the downregulation of ACE2 expression in SARS-CoV infections might play a causal role in SARS pathogenesis, especially in disease progression to ARDS.”21 Ultimately more research is needed in looking specifically at vitamin supplementation in COVID-19 in order to answer this question.
Vitamin D and DPP-4
There are multiple ways that vitamin D may be protective in COVID-19. It modulates the immune system to reduce inflammation, and it also induces the release of cathelicidins, which are wide-spectrum antimicrobial peptides that target bacteria, viruses, and fungi22. Another way vitamin D may have an impact has to do with dipeptidyl peptidase 4 (DPP4 aka CD26). It is known that the SARS-CoV2 virus targets ACE2 to infect the host. Recently a study using modelling of the structure of the SARS-CoV-2 virus predicted interaction via a docking mechanism of the virus and DPP4, which is the target for MERS, a related coronavirus23. It is possible that this is another mode of infection, although it remains to be proven.
DPP4 is expressed throughout the body and is involved in many processes, one of which has to do with blood sugar regulation. Higher plasma levels of DPP4 are found in metabolic syndrome, diabetes, obesity and aging, all of which are risk factors for more severe COVID-19 illness24. DPP4 inhibitors are a class of drugs used to treat diabetes, and they have inflammation-modulating and antifibrotic activity25. This class of drugs has also been shown to be beneficial in cardiovascular disease and to help reduce endothelial dysfunction26, which is an emerging symptom of concern in COVID-19. High DPP4 levels are associated with poor outcomes in hepatitis C, and vitamin D supplementation was shown to reduce DPP4 levels27. While the connection between DPP4, vitamin D, and COVID-19 are tentative at this point, it would be worthwhile to investigate28.
Vitamin D and Coagulation
Early on COVID-19 was thought to be primarily a lung disease, whereby certain lung cells were infected and destroyed, leading to inflammation, pneumonia, difficulty breathing and ultimately acute respiratory distress syndrome, requiring ventilation. Hyperinflammation appears to not only impact the lung but also contributes to increased coagulation of the blood29. This can lead to heart attack, stroke, pulmonary embolism, deep vein thrombosis – basically blockages of blood vessels anywhere in the body. This coagulopathy has a poor prognosis, and in one study, evidence of coagulation was much more prevalent in the COVID-19 patients who died than in those who survived30. The process of coagulation is complex, and in COVID-19, several factors most likely contribute to it, from hyperinflammation, increased levels of angiotensin II, and possible infection of ACE2 located within the blood vessels, contributing to endothelial injury31. Vitamin D plays an important role in hemostasis, which is the balance between the formation and disintegration of clots32. It is therefore possible that it could play a role in preventing coagulopathy in COVID-19.
Sufficient Vitamin D Status is Important for General Health
While early observational research shows an association between low vitamin D status and severe COVID-19 illness, it is unclear if insufficiency/deficiency plays a causal role or perhaps if the infection causes vitamin D depletion. There are currently 11 studies in the works to learn more about the effects of vitamin D supplementation (either alone or in combination with other nutrients and/or drugs) in COVID-19. What is currently known that is that vitamin D deficiency/insufficiency is common, and low vitamin D status is associated with many acute and chronic illnesses. “With all of the mounting evidence for a wide variety of health benefits associated with vitamin D sufficiency there is no downside to be improving everyone’s vitamin D status.”17 Therefore, if you are uncertain about your vitamin D status, live in the Pacific Northwest or other at risk latitudes, and/or fall into one of the groups commonly deficient, it may be worthwhile to have your status checked. Correcting vitamin D deficiency/insufficiency is easy, inexpensive, and safe to do.
Similar article:
Is Elderberry Safe in COVID-19?
Featured Photo by Michele Blackwell on Unsplash
REFERENCES:
1. Kalligeros M, Shehadeh F, Mylona EK, et al. Association of Obesity with Disease Severity among Patients with COVID-19. Obes (Silver Spring). 2020;April 20. doi:10.1002/oby.22859
2. Meng Y, Wu P, Lu W, et al. Sex-specific clinical characteristics and prognosis of coronavirus disease-19 infection in Wuhan, China: A retrospective study of 168 severe patients. PLOS Pathog. 2020;16(4):e1008520. doi:10.1371/journal.ppat.1008520
3. Panarese A, Shahini E. Letter: Covid-19, and vitamin D. Aliment Pharmacol Ther. 2020:993-995. doi:10.1111/apt.15752
4. Tian Y, Rong L. Letter: Covid-19 and vitamin D-authors’ reply. Aliment Pharmacol Ther. 2020;1:995-996. doi:10.1111/apt.15764
5. Jakovac H. COVID-19 and vitamin D-Is there a link and an opportunity for intervention? Am J Physiol Endocrinol Metab. 2020;318(5):E589. doi:10.1152/ajpendo.00138.2020
6. Hope-Simpson RE. The role of season in the epidemiology of influenza. J Hyg (Lond). 1981;86:35-47. doi:10.1017/S0022172400068728
7. Cannell JJ, Vieth R, Umhau JC, et al. Epidemic influenza and vitamin D. Epidemiol Infect. 2006;134(6):1129-1140. doi:10.1017/S0950268806007175
8. Urashima M, Segawa T, Okazaki M, Kurihara M, Wada Y, Ida H. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am J Clin Nutr. 2010;91(5):1255-1260. doi:10.3945/ajcn.2009.29094
9. Gruber-Bzura BM. Vitamin D and influenza—Prevention or therapy? Int J Mol Sci. 2018;19(2419):1-25. doi:10.3390/ijms19082419
10. Zhou Y, Luo B, Qin L. The association between vitamin D deficiency and community-acquired pneumonia: A meta-analysis of observational studies. Medicine (Baltimore). 2019;98(38):1-7. doi:10.1097/MD.0000000000017252
11. Ye Q, Wang B, Mao J. The pathogenesis and treatment of the `Cytokine Storm’ in COVID-19. J Infect. 2020. doi:10.1016/j.jinf.2020.03.037
12. Dancer RCA, Parekh D, Lax S, et al. Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS). Thorax. 2015;70(7):617-624. doi:10.1136/thoraxjnl-2014-206680
13. Han JE, Jones JL, Tangpricha V, et al. High dose Vitamin D administration in ventilated intensive care unit patients: A pilot double blind randomized controlled trial. J Clin Transl Endocrinol. 2016;4:59-65. doi:10.1016/j.jcte.2016.04.004
14. Rhodes JM, Subramanian S, Laird E, Anne Kenny R. Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North – supports vitamin D as a factor determining severity. Aliment Pharmacol Ther. 2020:1-4. doi:10.1111/apt.15777
15. Ilie PC, Stefanescu S, Smith L. The role of Vitamin D in the prevention of Coronavirus Disease 2019 infection and mortality. Aging Clin Exp Res. 2020. doi:10.21203/rs.3.rs-21211/v1
16. Lau FH, Majumder R, Torabi R, et al. Vitamin D Insufficiency is Prevalent in Severe COVID-19. medRxiv. 2020;(504):2020.04.24.20075838. doi:10.1101/2020.04.24.20075838
17. Holick MF. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. 2017;18(2):153-165. doi:10.1007/s11154-017-9424-1
18. Li YC, Qiao G, Uskokovic M, Xiang W, Zheng W, Kong J. Vitamin D: A negative endocrine regulator of the renin-angiotensin system and blood pressure. J Steroid Biochem Mol Biol. 2004;89-90:387-392. doi:10.1016/j.jsbmb.2004.03.004
19. Vaduganathan M, Vardeny O, Michel T, et al. Special Report: Renin – Angiotensin – Aldosterone System Inhibitors in Patients with Covid-19. N Engl J Med. 2020;382(17):1653-1659. doi:10.1056/NEJMsr2005760
20. Xu J, Yang J, Chen J, Luo Q, Zhang Q, Zhang H. Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system. Mol Med Rep. 2017;16(5):7432-7438. doi:10.3892/mmr.2017.7546
21. Kuba K, Imai Y, Penninger JM. Angiotensin-converting enzyme 2 in lung diseases. Curr Opin Pharmacol. 2006;6(3):271-276. doi:10.1016/j.coph.2006.03.001
22. Grant WB, Lahore H, McDonnell SL, et al. Evidence that vitamin d supplementation could reduce risk of influenza and covid-19 infections and deaths. Nutrients. 2020;12(4):1-19. doi:10.3390/nu12040988
23. Vankadari N, Wilce JA. Emerging WuHan (COVID-19) coronavirus: glycan shield and structure prediction of spike glycoprotein and its interaction with human CD26. Emerg Microbes Infect. 2020;9(1):601-604. doi:10.1080/22221751.2020.1739565
24. Barchetta I, Cavallo MG, Baroni MG. Letter to the Editor COVID-19 and diabetes : Is this association driven by the DPP4 receptor ? Potential clinical and therapeutic implications. Diabetes Res Clin Pract. 2020;163. doi:10.1016/j.diabres.2020.108165
25. Strollo R, Pozzilli P. DPP4 inhibition: preventing SARS‐CoV ‐2 infection and/or progression of COVID‐19? Diabetes Metab Res Rev. 2020;(1). doi:10.1002/dmrr.3330
26. Liu H, Guo L, Xing J, et al. The protective role of DPP4 inhibitors in atherosclerosis. Eur J Pharmacol. 2020;875:173037. doi:10.1016/j.ejphar.2020.173037
27. Komolmit P, Charoensuk K, Thanapirom K, et al. Correction of Vitamin D deficiency facilitated suppression of IP-10 and DPP IV levels in patients with chronic hepatitis C: A randomised double-blinded, placebo-control trial. PLoS One. 2017;12(4):1-14. doi:10.1371/journal.pone.0174608
28. McCartney DM, Byrne DG. Optimisation of Vitamin D Status for Enhanced Immuno-protection Against Covid-19. Ir Med J. 2020;113(4):58.
29. Henry BM, Vikse J, Benoit S, Favaloro EJ, Lippi G. Hyperinflammation and derangement of renin-angiotensin-aldosterone system in COVID-19: A novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis. Clin Chim Acta. 2020:167-173. doi:10.1016/j.cca.2020.04.027
30. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844-847. doi:10.1111/jth.14768
31. Belen-Apak FB, Sarıalioğlu F. Pulmonary intravascular coagulation in COVID ‑ 19 : possible pathogenesis and recommendations on anticoagulant/thrombolytic therapy. J Thromb Thrombolysis. 2020. doi:10.1007/s11239-020-02129-0
32. Mohammad S, Mishra A, Ashraf MZ. Emerging role of vitamin d and its associated molecules in pathways related to pathogenesis of thrombosis. Biomolecules. 2019;9(11):1-14. doi:10.3390/biom9110649