The COVID-19 pandemic caused by the novel coronavirus SARS-CoV-2 has infected millions of people worldwide and led to recommendations like many of us have never seen before. People are confused due to conflicting information and frustrated because they do not know who to believe. The issue of wearing masks is a good example. Early on, due to protective personal equipment (PPE) shortages of things like N95 respirators and surgical masks, it was recommended that the general public not wear masks. The rationale was that PPE should be conserved for healthcare workers on the frontline dealing with sick patients. Because it was thought that COVID-19 transmission mainly occurred when people were symptomatic, there would be little benefit for the general public to wear masks.
That changed on April 6, 2020, when the Center for Disease Control (CDC) began recommending that the general public start using cloth masks that could easily be made from materials that people already had on hand to prevent the spread COVID-19. However, mask-wearing guidelines from health authorities all over the world differed widely1, and even the World Health Organization (WHO) did not recommend the widespread use of masks until just recently. Because of these inconsistencies and changes in policies that look like flip-flopping, particularly in the US there has been doubt as to whether wearing a mask in public is likely to help reduce the spread of COVID-19. Therefore, I thought it would be useful to look into the medical literature for evidence that answers the question, “Does wearing a mask reduce the spread of infection, particularly SARS-CoV-2?”
Initial Objections to Widespread Mask-Wearing
Early objections to recommending widespread use of masks were that N95 respirators and surgical masks should be saved for healthcare workers due to their limited supply. There was also an assumption that non-medical or homemade masks would not be helpful, and – even worse – they might create a false sense of safety and cause people to touch their faces more and/or stop other preventative behaviors like social distancing and handwashing, which have been considered foundational behaviors in “flattening the curve”. However, Cheng et al point out that there does not appear to be any evidence “that wearing masks would mean other approaches to infection control would be overlooked.”2
How Is COVID-19 Spread?
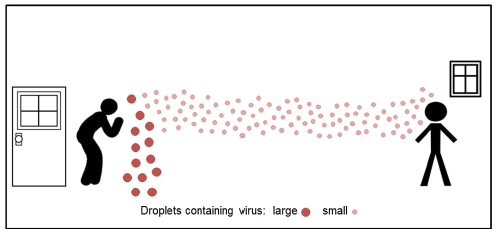
Since those early days, it has become clear that the virus can be spread when people are asymptomatic (they are infected but will never develop symptoms) or presymptomatic (they are infected and have not yet developed symptoms, but they will), with estimates that 46-55% of transmission occurs in the presymptomatic phase.3 In addition, the virus was thought to spread mainly through direct contact and respiratory droplets from coughing or sneezing. However, it is now clear that the virus can also be transmitted via aerosols that are released into the environment through talking and even just breathing.4 This means that someone who is infected but feels fine can be transmitting virus particles in the air just by breathing or talking without realizing that they are infectious. It is thought that by wearing masks in public, we can reduce COVID-19 transmission by reducing the amount of respiratory droplets and infectious aerosols that we are unknowingly putting into the environment. This is called “source control”, and so it is important to understand that the rationale for widespread mask-wearing is as much or more so about protecting others as it is about protecting ourselves from being exposed to this virus.2
COVID-19 Transmission Rate
The “reproductive number” describes the rate at which a disease is spread, and it is represented by “R0”, also called “R naught”. When R0 = 1, it means that an infected person will infect 1 other person. When R0 = 2, it means 1 infected person will go on to infect 2 people. Those 2 people will go on to infect 2 people each for a total of 4 new infections, and so on. In order for an infection to keep spreading in the environment, the R0 must be greater than 1. The R0 of SARS-CoV-2 has been estimated to be anywhere from 2.2 – 5.7.5 However, the measures introduced to “flatten the curve” have a big impact on the R0 because they are intended to minimize the opportunities for the virus to spread. This is a great resource that is tracking the R0 over time in different states.
Do Cloth Masks Work?
I have seen statements on social media that wearing masks does not work to reduce disease transmission, and so it is important to look at the evidence to see if this is true. I think some skepticism is valid because we all know that virus particles are very small – so small that we cannot see them with our naked eye. A cloth mask made with quilter’s cotton – like many homemade masks are – has a fairly coarse weave, and so it is logical to doubt that this would be able to filter out the virus particles. Something to remember is that these virus particles are traveling via large and small droplets, and these droplets can be filtered by fabric. A University of Reading professor of virology named Ian Jones said, “If an aerosol droplet hits the weave of the mask fabric rather than the hole it is clearly arrested. And lessening the aerosol dose chips away at the R0 and helps to slow the epidemic . . . They are not a cure but they address the longer flatter epidemic curve everyone is trying to achieve.”6 But let us not just take Jones’ word for it. Several researchers have looked at how well various fabrics filter particles.
Cloth Masks Can Provide Mechanical and Electrostatic Filtration
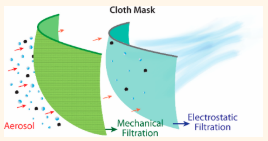
Konda et al. evaluated the filtration efficiency of cotton, flannel, chiffon, and silk fabrics with respect to aerosol droplets ranging from ~10 nm to ~10 µm, and they ran experiments with single layers, multiple layers and combinations of different fabrics.7 They found, not surprisingly, that fabric with a tighter weave like high thread count cotton (600 threads per inch – TPI) performed better than low thread count (quilter’ cotton ~80 TPI) at mechanically filtering out particles. However, they found that fabrics like silk, chiffon (90% polyester and 10% spandex), and flannel had electrostatic properties and were able to filter smaller particles (10 nm – 6 µm), particularly at low velocities similar to that of breathing. They found that using multiple layers and combining different fabrics increased efficiency. For example, with two layers of 600 TPI cotton and two layers of silk, filtration efficiency was 94% for particles under 300 nm and 98.5% for particles larger than 300 nm. This combination actually filtered smaller particles better than the N95 respirators, which are certified to filter 95% of particles larger than 0.3 µm. This is particularly relevant, since coronarviruses measure 0.06-0.04 µm.8 However, the authors note that the fit of the mask, regardless of type or material, plays a big role in how effectively it filters, and poor fit (i.e. gaps around mask edges) can reduce filtration efficacy by over 60%.
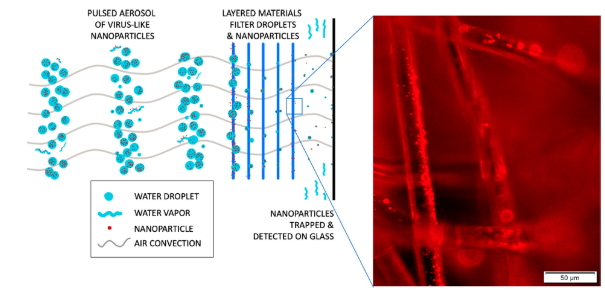
In another study, Lustig et al. studied the filtration efficacy of 70 different common fabrics where they pulsed aerosol droplets containing fluorescent virus-like nanoparticles across the different materials at an air convection similar to that of forceful breathing.9 Nanoparticles were collected and measured on a glass on the other side of the material, and the transmission rates were compared to that of an N95 mask. They found that certain combinations like 1) two layers of white denim with 2 layers of OLY-FUN (65 GSM polypropylene nonwoven fabric) and 2) two layers of Kona quilting cotton with 4 layers of OLY-FUN actually filtered more particles than the N95. They concluded by recommending that masks have different layers of woven and nonwoven fabrics, including layers that absorb as well as repel water. For absorbent layers, terry cloth towel, quilting cotton and flannel were effective. The nonwoven material recommendations were polypropylene, polyester and polyaramid. These authors also stressed that the fit of the mask must be snug so that aerosols do not enter through gaps around the mask edges, and they also mention that the mask must not touch the lips.
Does Widespread Mask-Wearing Reduce Disease Transmission?
These two filtration studies show that cloth masks have the potential to be effective filters, but the authors are clear about the fit being important. I am sure we have all witnessed gapping masks, and masks not covering everything they are supposed to. That is the real-world, where compliance and efficiency are not 100%, so it is helpful to look at real-world applications where masks have been used to prevent disease.
In a randomized controlled trial, breath was collected from people with respiratory tract infections who were randomized to wearing a face mask or not wearing a face mask, and the conclusion was that surgical masks reduced the amount of coronavirus detected in respiratory droplets and aerosols.10 A meta-analyses including 21 studies with 8686 participants looked at whether use of masks by healthcare workers and non-healthcare workers prevented respiratory infections and concluded that the “risk of influenza, SARS, and COVID-19 infection were reduced by 45%, 74%, and 96% by wearing masks, respectively, which were consistent with previous meta-analyses during the SARS outbreaks.”11
How Taiwan, Hong Kong and S. Korea Controlled COVID-19
Taiwan reported its first case of COVID-19 on January 21, 2020. Being so close to China with many of its citizens working or residing in China, it was at major risk of the virus spreading within its population. However, early on there was a government effort to increase surgical masks supply and make these available at low cost to the general public.12 Along with affordable medical care for people who suspected they might be ill with COVID-19, wearing masks was a major piece of Taiwan’s strategy to limit the spread of the disease, and as of this writing, they have only had 448 confirmed cases and 7 deaths.
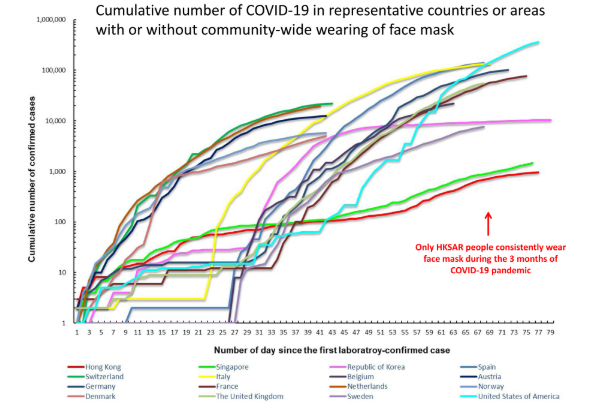
Cheng et al found that in Hong Kong, voluntary community-wide mask wearing was about 96.8%, and the incidence of disease within the first 100 days from first infection was significantly lower than in countries that did not have widespread mask use.13
South Korea is another country that has been able to reign in the spread of the virus. In February, S. Korea experienced a rapid increase in cases but quickly implemented aggressive testing, tracing, and treating, along with other behavioral measures like social distancing, handwashing, and wearing masks.14 Mask-wearing by the general public was reported to be anywhere from 63.2-94% and is considered to be one of the most effective measures that they used to reduce spread of the disease.
Mathematical Models of Mask-Use in the United States
Ngonghala et al. used a mathematical model to look at the effects of non-pharmaceutical interventions (NPIs) like social distancing and mask-wearing to reduce the burden of COVID-19 in the US.15 They ran models looking at mask efficiency as well as mask-wearing compliance. They found that if 70% or more of the population wore highly efficient masks, like surgical masks, then the elimination of COVID-19 is possible. Even with masks that are inefficient like 2 layer cotton masks, hospitalizations could be reduced by up to 64% if at least 75% of the population wore them.
Another study by Lyu and Wehby looked at 15 states that had mask-wearing mandates issued by their governors and compared the COVID-19 growth rate to states that did not have mask mandates.16 They looked at trends during five-day periods starting 5 days before the mandate all the way to 20 days after the mandate. They conclude that “the daily case rate declines by 0.9, 1.1, 1.4, 1.7, and 2.0 percentage-points within 1–5, 6–10, 11–15, and 16–20, and 21+ days after signing, respectively.” On the whole, they estimate that the mask mandates in these states may have prevented anywhere from 230,000-450,000 cases.
Face Masks Are an Important Strategy to Reduce Disease
The recommendation to wear face masks as a strategy to reduce the daily cases of COVID-19 has been controversial. Certain Asian countries that have had previous experience with epidemics like SARS and MERS have had high compliance with mask mandates with many people voluntarily wearing them. However, in the US, this recommendation has been viewed by some as an infringement on personal freedom. Considering that the US only makes up about 4.25% of the world’s population but accounts for roughly 26% of the world’s cases, we have to acknowledge that the pandemic is not well-controlled in this country. It is time to start looking at and implementing strategies that have been used in other countries to successfully reduce the spread of this disease. Americans are fiercely independent, but we need to realize that our actions impact others, and wearing masks is a simple and effective public health strategy meant to benefit our community at large. Wearing masks in public is not meant to be a magic bullet that we pin all of our COVID-19 hopes on, but combined with continued social distancing, handwashing, and other health-promoting activities, it has shown to play an important role in reducing COVID-19 cases, hospitalizations, and deaths.
Other COVID-19 articles:
Are Low Vitamin D Levels a Risk for Serious COVID-19?
Is Elderberry Safe in COVID-19?
Featured Photo by Vera Davidova on Unsplash
REFERENCES:
1. Laestadius L, Wang Y, Ben Taleb Z, Kalan ME, Cho Y, Manganello J. Online National Health Agency Mask Guidance for the Public in Light of COVID-19: Content Analysis. JMIR Public Heal Surveill. 2020;6(2):e19501. doi:10.2196/19501
2. Cheng KK, Lam TH, Leung CC. Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity. Lancet. 2020. doi:10.1016/S0140-6736(20)30918-1
3. He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26(5):672-675. doi:10.1038/s41591-020-0869-5
4. Morawska L, Cao J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environ Int. 2020;139(April):105730. doi:10.1016/j.envint.2020.105730
5. Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2. Emerg Infect Dis. 2020;26(7):1-8. doi:10.3201/eid2607.200282
6. Mahase E. Covid-19: What is the evidence for cloth masks? BMJ. 2020;369(April):m1422. doi:10.1136/bmj.m1422
7. Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. ACS Nano. 2020. doi:10.1021/acsnano.0c03252
8. Goh Y, Tan BYQ, Bhartendu C, Ong JJY, Sharma VK. The face mask: How a real protection becomes a psychological symbol during Covid-19? Brain Behav Immun. 2020;(May):0-1. doi:10.1016/j.bbi.2020.05.060
9. Lustig SR, Biswakarma JJH, Rana D, et al. Effectiveness of Common Fabrics to Block Aqueous Aerosols of Virus-like Nanoparticles. ACS Nano. 2020. doi:10.1021/acsnano.0c03972
10. Leung NHL, Chu DKW, Shiu EYC, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26(5):676-680. doi:10.1038/s41591-020-0843-2
11. Liang M, Gao L, Cheng C, et al. Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta-analysis. Travel Med Infect Dis. 2020. doi:10.1016/j.tmaid.2020.101751
12. Yi-Fong Su V, Yen Y-F, Yang K-Y, et al. Masks and medical care: Two keys to Taiwan’s success in preventing COVID-19 spread. Travel Med Infect Dis. 2020. doi:10.1016/j.tmaid.2020.101780
13. Cheng VC, Wong S, Chuang VW, et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect. 2020:107-114. doi:10.1016/j.jinf.2020.04.024
14. Lim S, Yoon H Il, Song K-H, Kim ES, Kim H Bin, Fidsa. Face Masks and Containment of Coronavirus Disease 2019 (COVID-19): Experience from South Korea. J Hosp Infect. 2020. doi:10.1016/j.jhin.2020.06.017
15. Ngonghala CN, Iboi E, Eikenberry S, et al. Mathematical assessment of the impact of non-pharmaceutical interventions on curtailing the 2019 novel Coronavirus. Math Biosci. 2020;325(May):108364. doi:10.1016/j.mbs.2020.108364
16. Lyu W, Wehby GL. Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US. Health Aff (Millwood). 2020;39(8):1-7. doi:10.1377/hlthaff.2020.00818