Naturopathic medicine has a longstanding tradition of recognizing that gut health is central to overall health, and this is now being reflected in the medical literature, especially with the vastly expanding research regarding the importance of the gut microbiome. However, many people suffer from irritable bowel syndrome or other digestive complaints, sometimes not even knowing that what they are experiencing is not actually “normal”. If someone is experiencing digestive problems on a regular or even semi-regular basis, it is possible that they suffer from IBS, which can negatively impact a person’s quality of life.
What is IBS?
IBS stands for “irritable bowel syndrome”, which basically describes how it feels. The main symptoms of IBS are chronic abdominal pain that is accompanied by “altered bowel habits” like constipation, diarrhea, or a combination of constipation and diarrhea. IBS is considered a functional digestive disorder because the symptoms exist without an easily detectable cause [1]. Basically, this is a diagnosis that is given when other disease is not found. For example, the labs and imaging that are done to rule out diseases like celiac disease, Crohn’s disease, ulcerative colitis, or gastroenteritis (to name a few) will be normal. In addition, other criteria need to be met. The Rome IV criteria are the most commonly used to diagnose IBS.
Rome IV Criteria for IBS
In IBS, there is recurrent abdominal pain, which typically occurs at least one day per week for the past three months, and the abdominal pain is associated with at least two of the following:
- The pain is related to defecation.
- There is a change in frequency of bowel movements.
- There is a change in the appearance/form of the stool.
Who is Affected by IBS?
IBS affects about 10-15% of people in North America, with a higher prevalence in women. Many people do not seek medical attention for this disorder, and it is estimated that about 40% of people who suffer from IBS do not have an official diagnosis [2]. Even though many people do not seek help for IBS, this condition makes up 25-50% of referrals to gastroenterologists. IBS is also associated with conditions like fibromyalgia, chronic fatigue syndrome as well as depression and anxiety.
IBS and SIBO
The underlying cause for IBS remains hard to pin down. Very likely this is a condition that can be caused by variety of factors. One of the factors appears to be alterations in the gut microbiome in terms of which microorganisms are present as well as where in the digestive tract they are located. IBS and small intestinal bacterial overgrowth (SIBO) share many of the same symptoms, like abdominal pain, diarrhea, constipation, or mixed diarrhea/constipation. A meta-analysis showed that SIBO is present in 31.0% of IBS cases [3]. In SIBO, there is an overgrowth of normal bacteria in the small intestine, which leads to symptoms and potentially to malabsorption of nutrients and intestinal inflammation. The easiest way to check for SIBO is with a glucose or lactulose breath test. You can read more about SIBO here.
IBS and Food Sensitivities
IBS symptoms often are worse after eating certain foods. This can certainly be the case in SIBO when certain foods are fermented by the bacteria in the small intestine, causing gas, bloating and pain. However, food sensitivities are starting to be acknowledged as a potential contributors to IBS [1]. Food sensitivities are different from food allergies, which are caused by an IgE immune response. Food sensitivities are usually caused by an IgG response to foods, and the onset of symptoms usually takes noticeably longer than an IgE response. Studies have found that eliminating foods to which a person is sensitive can improve IBS symptoms. The gold standard in determining food sensitivities is an elimination diet. Food sensitivities can also be assessed with serum IgA and/or IgG food sensitivity testing. While this type of testing has not been validated, people often feel better when they eliminate the foods identified on food sensitivity panels for a period of time.
IBS and Stress
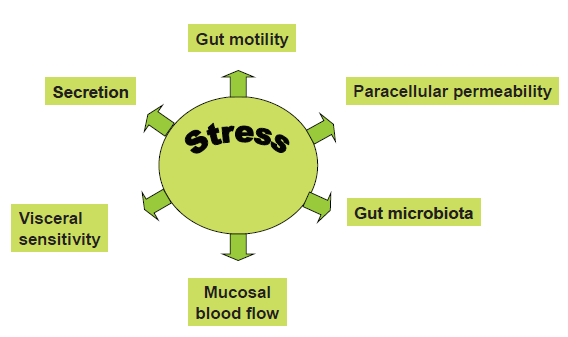
The International Foundation of Gastrointestinal Disorders has a website with loads of information about IBS. This is a great resource, but in their “Facts About IBS”, they say that although stress can exacerbate IBS, it does not cause it. As mentioned before, there are various and often multiple causes for a person’s IBS, and CHRONIC stress could certainly be a cause. There are many ways that stress can cause digestive problems by changing motility (how quickly your food moves through your system), increasing visceral hypersensitivity (leading to higher perceived pain with intestinal distension), increasing intestinal permeability (leaky gut), by negatively impacting the gut microbiota, and by reducing blood flow to the intestinal mucosa (causing impaired digestion and tissue regeneration) [4]. In a recent review, the authors described IBS as a disease of gut-brain axis dysregulation [5] where inflammatory changes appear to be brought on through the chemistry of stress. Therefore, stress management is an important target in IBS.
What to do About IBS?
There are many ways to address IBS like dietary and lifestyle changes, stress management strategies, antibiotics, probiotics, prokinetics, immunomodulators, as well as drugs and supplements that target symptom relief. However, as always, it is important to identify the root cause or causes of IBS, and this will be different in each person. A careful history along with appropriate lab testing will help to identify a treatment plan that is best suited for that particular person. Despite being common, IBS is not normal and can seriously impact a person’s quality of life in a negative way.
If you suffer from IBS or other digestive complaints, Dr. McManus is accepting new patients and can help uncover the root cause of these symptoms. Feel free to schedule a complimentary 15-minute discovery call or visit with her at Kirkland Natural Medicine by calling 425-448-3232.
References
| [1] | A. Wald MD, “Pathophysiology of irritable bowel syndrome,” UpToDate, 03 Sep 2020. [Online]. Available: https://www.uptodate.com/contents/pathophysiology-of-irritable-bowel-syndrome. |
| [2] | A. Wald MD, “Clinical manifestations and diagnosis of irritable bowel syndrome in adults,” UpToDate, 24 Feb 2021. [Online]. Available: https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-irritable-bowel-syndrome-in-adults. |
| [3] | W. Takahura and M. Pimental, “Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome – An Update,” Front. Psychiatry, vol. 11, no. 664, 2020. |
| [4] | P. Konturek, T. Brzozowski and S. Konturek, “Stress and the Gut: Pathophysiology, Clinical Consequences, Diagnostic Approach and Treatment Options,” J Physiol Pharmacol., vol. 62, no. 6, pp. 591-9, 2011. |
| [5] | M. Casado-Bedmar and A. Keita, “Potential neuro-immune therapeutic targets in irritable bowel syndrome,” Therap Adv Gastroenterol, vol. 13, pp. 1-15, 2020. |
