If you have ever suffered from chronic hives, you know how miserable they can be. Hives are raised, red areas on the skin that can be very itchy, making a person miserable and negatively affecting sleep and overall quality of life. Up to 20% of people experience hives sometime during their lifetime. When hives last for less than 6 weeks, the condition is called acute urticaria. When longer than 6 weeks, it is called chronic urticaria. Individual hives generally show up in groups anywhere on the body and usually resolve within 24 hours but often are replaced by new ones. Hives are caused when mast cells, a type of immune cell, that are in the skin become activated and release histamine. The histamine causes the swelling, redness, and itchiness. The first line of treatment for CSU is second-generation H1 antihistamines1, but for many people this only gives partial relief, and some people might not experience any change in symptoms. Furthermore, this treatment is mainly addressing the symptoms and does not address why these mast cells are getting activated in the first place.
What Causes Acute and Chronic Hives?
Acute urticaria is typically caused by an infection or allergic response to a food or environmental allergen. Chronic urticaria can be divided into two categories. “Chronic inducible urticaria” accounts for 20% of cases and is caused by something like sunlight, heat, cold, pressure, vibration. The remaining 80% of cases fall into the category of “chronic spontaneous urticaria”, and the trigger that activates the mast cell is unknown, which is why it is also called “chronic idiopathic urticaria”. Chronic spontaneous urticaria (CSU) is rarely caused by an environmental allergen, but certain things like stress, lack of sleep, NSAIDs, alcohol, heat, and tight clothing can make the symptoms worse. Unfortunately, because it can be extremely itchy and uncomfortable, CSU often interrupts sleep and causes stress, creating a vicious cycle.
Who Is Affected by Chronic Spontaneous Urticaria?
CSU occurs in about 1% of the adult population2, and it is more common in adults than children3 and in women than men4. However, since the early 1900s, there has been a link between chronic hives and autoimmune disease. In the 1980s, Leznoff et al. identified that autoimmune thyroid disease in particular was more common in people suffering from chronic urticaria5 than people without CSU, but the importance of this association has not been understood. Researchers have asked whether thyroid autoimmunity causes CSU in some people, or is it simply something unrelated that just happens to occur alongside chronic hives?
Autoimmune Thyroid Disease
Autoimmune thyroid disease can lead to hypothyroidism or hyperthyroidism. Hypothyroidism can cause symptoms like fatigue, weight gain, depression, constipation, cold intolerance, joint pain, and dry skin. Hyperthyroidism, on the other hand, can cause anxiety, irritability, hyperactivity, mood swings, diarrhea, racing heart rate, and insomnia. Hashimoto’s disease is the most common reason for hypothyroidism in the US, although in the earlier stages a person might fluctuate between a hypo- and hyperthyroid state. Graves’ disease causes hyperthyroidism and is less common than Hashimoto’s.
In autoimmune thyroid disease, there are elevated thyroid antibodies to one or more of the following: thyroperoxidase (TPO), thyroglobulin (Tg), and/or the TSH receptor (TSH-R). It is important to know that thyroid autoimmunity is common, affecting approximately 3-6% of the population6 and running as high as 15.3% in adult women7. Furthermore, the anti-TPO antibody, which is the most common thyroid antibody in both Hashimoto’s and Graves’ disease, can be elevated up to 5-7 years and possibly even more before a person begins to experience thyroid hormone imbalance8. Even when a person suffers from thyroid dysfunction, the conventional screening does not typically include labs to identify thyroid antibodies, so the people who are affected by thyroid autoimmunity are often not aware of it.
The Connection Between Chronic Hives and Autoimmune Thyroid Disease
Quite a few studies have looked at whether autoimmune thyroid disease occurs more often in people suffering from CSU vs. healthy controls. A review of 24 studies found that the prevalence of antithyroid antibodies in patients with CSU ranged from 3.7-37.1%4, which is higher than in the general population (see above). They also found that anti-TPO IgG was elevated more than any other thyroid antibody and that Hashimoto’s was more common in CSU than Graves’.
How Does Thyroid Autoimmunity Cause Chronic Hives?
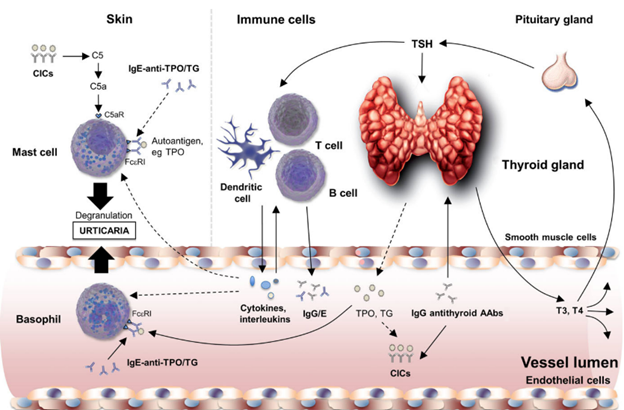
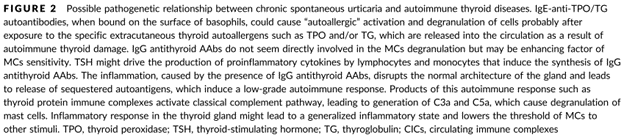
It is not clear if thyroid autoimmunity directly causes CSU, but there are several proposed mechanisms. One thought is that because thyroid autoimmunity involves heightened immune activity at the thyroid, it creates a low level of inflammation throughout the body. This in turn reduces the reactivity threshold of mast cells, allowing them to degranulate and release histamine more readily9. It has also been proposed that thyroid tissue destruction results in the activation of complement, which is a part of the innate immune system, and which can cause mast cell degranulation10.
Another thought is that the TSH hormone might play a role9. TSH is released from the pituitary gland and binds to the thyroid to stimulate it to make thyroid hormone. TSH generally rises when the brain senses a low level of thyroid hormones circulating in the blood, and conversely, it lowers when circulating thyroid hormones are high. TSH has some similarities with cytokines, which are chemicals released from immune cells, often involved in the process of inflammation. Furthermore, TSH does not just bind to the thyroid but can bind directly to immune cells, and so it can participate in immune activation11.
There are 5 different types of antibodies: IgA, IgD, IgE, IgM, and IgG. IgG antibodies are the most abundant and are involved in the learned immune response to infection and to autoimmunity. IgE antibodies are much less common and are involved with parasite infections and allergies. While antithyroid IgG antibodies do not appear to directly activate mast cells in CSU6, several studies have identified the presence of anti-TPO IgE antibodies in some CSU patients that can bind to mast cells and basophils, which can both release histamine12,13. These studies also found that people with anti-TPO IgE had significantly higher level of anti-TPO IgG antibodies. Not everyone with CSU has these anti-TPO IgE antibodies, but when they are present, they appear to play a causal role. ”IgE to TPO plays a pathogenic role in cellular effector activation and skin exacerbation in a subgroup of CSU patients, and this effect can be transferred to healthy subjects.”12
Levothyroxine for the Treatment of CSU?
Over the years there have been case studies and research trials that have looked at treating people suffering from CSU who also had some form of thyroid autoimmunity and/or thyroid dysfunction with drugs/hormones appropriate for their thyroid condition. There have been mixed results with some people showing complete remission of their CSU to others showing no change in their urticarial symptoms. For example, two case studies detailed how two different patients with CSU were diagnosed with elevated thyroid antibodies and hypothyroidism. They were treated with levothyroxine, which normalized their thyroid function and resolved the urticaria. Both cases remained symptom free at follow-up.14,15
A study from 2005 by Aversano et al. looked at 20 women who were diagnosed with CSU and thyroid autoimmunity to see how they would respond to l-thyroxine (aka levothyroxine) treatment11. While all the subjects were positive for thyroid antibodies, only 8 women were hypothyroid with an elevated TSH and the other 12 had normal thyroid function and normal TSH. All subjects were treated with thyroid hormone replacement until their TSH level was suppressed to <0.3 µIU/ml. The results showed that 16 of the 20 subjects had a strong improvement in their urticarial symptoms by 12 weeks, and there was a large decrease in the levels of thyroid antibodies.
While CSU and thyroid autoimmunity are less common in children and adolescents, Levy et al. wanted to see if there was a connection with autoimmune thyroid disease and CSU in this population3. Their study included 187 children between 6-18 years of age, who had been referred for CSU. Antithyroid antibodies were found in 8 out of 187, and three of these children were hypothyroid. These 3 were then treated with levothyroxine, but there was no remission in the urticaria. The authors concluded that levothyroxine treatment has no impact on the course of CSU.
These positive and negative studies are two small examples of some of the research that has been done. However, in 2017, Kolkhir et al. published a systematic review of 102 studies, addressing multiple aspects of CSU and thyroid autoimmunity, including whether CSU in the presence of thyroid antibodies can improve with levothyroxine or other thyroid drugs, and they found strong evidence that it could4. They caution, however, that there have not been randomized, double-blind, placebo-controlled studies with levothyroxine and CSU. Because up to 50% of CSU cases can experience spontaneous remission, without being able to compare the treatment to placebo, it is unclear whether the positive studies were due to the treatment or simply due to time.
CSU: a Clue for Thyroid Autoimmunity
It is agreed that chronic urticaria is caused by activated mast cells degranulating and releasing histamine. In chronic spontaneous urticaria, which accounts for 80% of chronic urticaria cases, the trigger for that mast cell degranulation is considered to be unknown. Most likely, this is a condition that includes a variety of unidentified triggers; however, research has shown a definite correlation with thyroid autoimmunity in a significant percentage of CSU sufferers. While thyroid hormone replacement studies have had mixed results, there is strong evidence that in the appropriate people, thyroid disease treatment can improve CSU. In any case, researchers strongly urge that people who suffer from CSU should be investigated for thyroid autoimmunity, particularly since silent thyroid autoimmunity frequently leads to thyroid dysfunction over time. In addition, while there is no cure for autoimmunity, there are many ways besides pharmaceuticals to address it and potentially bring it into remission. It is possible that by reducing autoimmune activity in the body and lowering overall systemic inflammation, the mast cells will become less reactive.
Even though the cause for CSU is considered to be “idiopathic”, it does not mean that there is not an actual cause. Based on the research, thyroid autoimmunity, which is underdiagnosed, appears to be a significant cause of CSU for some people. Therefore, chronic spontaneous urticaria with no identified trigger should be a signal to assess for thyroid autoimmunity because this might help identify the root cause of the chronic hives, leading to better outcomes for a condition that leads to significant suffering and which is often difficult to treat.
For more information, here is an article about by the American Academy of Dermatology Association about 10 ways to get relief from chronic hives.
More about autoimmune disease.
REFERENCES:
1. Schaefer P. Acute and Chronic Urticaria: Evaluation and Treatment. Am Fam Physician. 2017;95(11):717-724. http://www.ncbi.nlm.nih.gov/pubmed/28671445.
2. Zuberbier T, Maurer M. Urticaria: Current opinions about etiology, diagnosis and therapy. Acta Derm Venereol. 2007;87(3):196-205. doi:10.2340/00015555-0240
3. Levy Y, Segal N, Weintrob N, Danon YL. Chronic urticaria: Association with thyroid autoimmunity. Arch Dis Child. 2003;88(6):517-519. doi:10.1136/adc.88.6.517
4. Kolkhir P, Metz M, Altrichter S, Maurer M. Comorbidity of chronic spontaneous urticaria and autoimmune thyroid diseases: A systematic review. Allergy Eur J Allergy Clin Immunol. 2017;72(10):1440-1460. doi:10.1111/all.13182
5. Leznoff A, Josse R, Denburg J, Dolovich J. Association of chronic urticaria and angioedema with thyroid autoimmunity. Arch Dermatol. 1983;119(8):636-640. doi:10.1001/archderm.1983.01650320010007
6. Mozena JD, Tĩana A, Negri J, Steinke JW, Borish L. Lack of a role for cross-reacting anti-thyroid antibodies in chronic idiopathic urticaria. J Invest Dermatol. 2010;130(7):1860-1865. doi:10.1038/jid.2010.35
7. Rodríguez Y, Rojas M, Monsalve DM, et al. Latent autoimmune thyroid disease. J Transl Autoimmun. 2020;3(January). doi:10.1016/j.jtauto.2020.100038
8. Hutfless SM, Matos P, Talor M V., Caturegli P, Rose NR. Significance of prediagnostic thyroid antibodies in women with autoimmune thyroid disease. J Clin Endocrinol Metab. 2011;96(9). doi:10.1210/jc.2011-0228
9. Rumbyrt JS, Katz JL, Schocket AL. Resolution of chronic urticaria in patients with thyroid autoimmunity. J Allergy Clin Immunol. 1995;96(6):901-905. doi:10.1016/S0091-6749(95)70226-1
10. Dreskin SC, Andrews KY. The thyroid and urticaria. Curr Opin Allergy Clin Immunol. 2005;5(5):408-412. doi:10.1097/01.all.0000182546.83465.5a
11. Aversano M, Caiazzo P, Iorio G, Ponticiello L, Laganá B, Leccese F. Improvement of chronic idiopathic urticaria with L-thyroxine: A new TSH role in immune response? Allergy Eur J Allergy Clin Immunol. 2005;60(4):489-493. doi:10.1111/j.1398-9995.2005.00723.x
12. Sánchez J, Sánchez A, Cardona R. Causal relationship between Anti-TPO IgE and chronic urticaria by in vitro and in vivo tests. Allergy, Asthma Immunol Res. 2019;11(1):29-42. doi:10.4168/aair.2019.11.1.29
13. Altrichter S, Peter HJ, Pisarevskaja D, Metz M, Martus P, Maurer M. Ige mediated autoallergy against thyroid peroxidase – a novel pathomechanism of chronic spontaneous urticaria? PLoS One. 2011;6(4):e14794. doi:10.1371/journal.pone.0014794
14. Selvendran SS, Aggarwal N. Chronic urticaria and thyroid autoimmunity: a perplexing association. Oxford Med Case Reports. 2018;2018(2):61-63. doi:10.1093/omcr/omx099
15. Shahbaz A, Senapathi SH, Aziz K, Umair M, Khalid A, Sachmechi I. Improvement of Chronic Idiopathic Urticaria With Levothyroxine: A Case Report and Review of Literature. Cureus. 2018;10(8):8-11. doi:10.7759/cureus.3209